Let’s have a conversation about mental health
- Executive Summary
- Why we are talking about mental health
- Understanding the challenge
- Starting well
- Living well
- Ageing well
- Recommendations 2022/23
- Review of 2021/22 recommendations
- References and further reading
Executive summary
One in six adults will experience a common mental health problem in their lifetime, and poor mental health is the second leading cause of ill health in England. Torbay is ranked the most deprived local authority in the South West and faces challenges to the mental health and wellbeing of its population which the COVID-19 pandemic has only made worse. Since the pandemic, there is evidence of an increase in anxiety and low wellbeing, with depressive symptoms having a particular impact on young people and women. There are also indications that the experience of depression amongst those with a challenging financial situation has significantly increased.
The lockdowns have made existing socio-economic inequalities worse with specific groups particularly affected (see chapter 2).
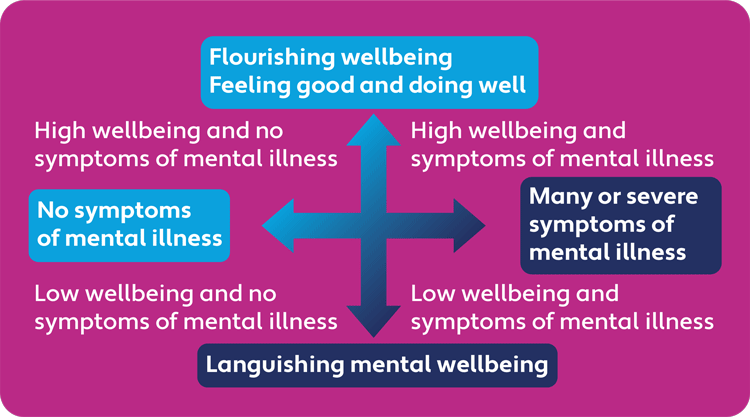
Good or poor mental health is more than the presence or absence of a diagnosis. Achieving and maintaining good mental health also requires good wellbeing. To achieve good mental health and wellbeing we need to be resilient, continually developing and applying learnt skills to minimise the impact of stress. Tackling poor mental health and wellbeing requires an approach that takes account of the whole person and their social context. Aspects such as belonging, identity, social connection, and purpose are central, as is the environment in which people live.
Torbay has the third highest number of school age children needing Social, Emotional and Mental Health interventions and self-harm remains a key area of concern. Torbay has the second highest number of referrals to social care services in the region with the highest rates of children in care.
Before the pandemic, Torbay residents generally reported positive wellbeing, however almost one in four said they had high anxiety levels. Around one in five residents reported having a common mental disorder such as anxiety or depression. Selfharm and suicide rates were significantly higher than the national average.
Since the start of the pandemic, the mental health and wellbeing of the population has worsened. People have experienced new levels of distress, anxiety and depression which they had not experienced before. Problems sleeping and disordered eating have become more prevalent. People with a mental health diagnosis have found that their condition has got worse. The pandemic has caused a rise in external stressors, such as job loss, debt, lack of social contact and domestic abuse, which then impact upon people’s ability to cope, especially if they already have an underlying mental health condition.
Torbay has an ageing population, creating complex challenges for the community and the agencies who seek to support individuals with their mental health and wellbeing. For older members of the community, COVID-19 has led to enforced inactivity and a loss of physical fitness, increased social isolation and separation from family and friends as well as fears of going out again for work, hobbies, shopping or socialising.
While there are many examples of community partnership, working collaboratively with multiple and diverse agencies to support and promote good mental health; pausing or cancellation of services and interventions during the pandemic has contributed to people with existing and new needs not getting the help they need in a timely manner.
For all partners across Torbay, supporting the mental health of our staff, clients, patients, students, and communities, is critically important. It is a time of real need, but also a time of real opportunity. COVID-19 has sharpened our understanding of our mental wellbeing. Never has it been more evident that ‘mental health is everyone’s business’. Without good mental health, schools, hospitals, businesses and communities suffer. With good mental health, we all thrive.
Recommendations for 2022
Recommendation 1
Ensure mental health and suicide prevention remain a priority for strategic partners across Torbay.
Recommendation 2
Drive continuous improvement in Children and Young People’s mental health outcomes through partnership with families and communities.
Recommendation 3
Implement the Torbay suicide and self-harm prevention plan with the aim of stabilising and reducing rates of suicide and selfharm across the Bay.
Recommendation 4
Incorporate mental health and wellbeing into the Multiple Complex Needs alliance from 2022
Recommendation 5
Support the creation of mental health promoting communities through community development, training, safe spaces and peer support.
Recommendation 6
Promote and support workplace wellbeing in all sectors across Torbay.
Recommendation 7
Promote approaches which tackle physical and mental wellbeing together especially physical activity and green spaces to improve wider health and wellbeing.
Recommendation 8
Collaborate with stakeholders to better understand needs and gaps in mental health to inform future planning and quality improvement.
Why we are talking about mental health
When the news came at the end of 2019 that a new illness had emerged in China, we had no way of knowing that it would dominate global affairs for more than a year and counting. In her final annual report, my predecessor documented the first year of our response to COVID-19 in Torbay. The fact that a year later I am starting my first report with reference to the pandemic speaks to its persistence.
Despite significant advances such as a successful mass vaccination programme and a better understanding of the clinical treatment of COVID-19, there is still uncertainty about how the pandemic will evolve, and the threat of new variants remains. At a time when supportive relationships and social contact were most important for our resilience, we were unable to meet our friends and extended family. At various points over the past months, we have not felt in control of important aspects of our everyday lives. It is hardly surprising that our mental health has been affected.
There was an increasing openness about mental health before the COVID-19 pandemic and that awareness has continued. However, a superficial sense that we are “all in this together” can divert attention from those who have experienced the impact of the pandemic and national restrictions to a greater extent than most. These include people with pre-existing mental health problems. COVID-19 exposed the inequalities that already existed, then widened and deepened them. While many will have the resilience to bounce back, there are those who will continue to experience the adverse effects of the pandemic well into the future, long after the majority have moved on.
My aim in highlighting mental health in this report is to bring a population perspective to the issue. The experience of mental health is highly individual and two people faced with similar circumstances may have very different responses. However, patterns emerge when we examine how a disease behaves in a population. To take an example, each suicide is unique. The factors that lead someone to take their life at a specific point in time will apply only in that instant. However, looking at suicides over time we note an increase in Torbay and when we compare our rates with other similar areas they are consistently high. This indicates that whatever the circumstances accounting for individual cases, there are factors operating across the population that is contributing to high suicide rates in Torbay. Reducing suicide requires a focus on the causes in each case as well as on the causes of those causes, such as the social and economic factors that make someone believe that taking their life is their only option.
Our ability to describe the patterns of mental health in the population depends on the measures we have at our disposal. We traditionally collect routine information on disease and deaths rather than measuring positive wellbeing in populations. Mental illness encompasses many diagnostic categories and each illness has its own spectrum of severity. We may all have experienced a depressed mood and other symptoms of depression at some point but this does not necessarily mean that we meet the criteria for depression.
Feeling “down” on a given day has as much to do with a diagnosis of major depression as the occasional headache has with having a brain tumour. This is where a population perspective can add value in helping us to understand the full extent of mental ill health.
A population perspective also helps to differentiate between the spectrum of mental illness and mental wellbeing – the positive dimension of mental health. Faced with similar adverse circumstances, some people will demonstrate resilience and others will experience negative consequences. We know that children who are exposed to traumatic experiences are at increased risk for poor mental health outcomes in later life. However, not every child has those negative consequences and protective factors are also important. Identifying the intrinsic and extrinsic factors that build resilience and protect against adversity can help people to maintain positive mental wellbeing in the face of mental or physical illness. An objective of public health is to reduce threats to population health, but helping people to be resilient despite these threats is also crucial.
Positive mental wellbeing affects all aspects of life and all aspects of life influence our mental wellbeing. If we feel that we have control over our lives, have a sense of purpose and supportive relationships, we are more likely to have a positive outlook when faced with challenges and we are more likely to find solutions to our problems. Positive wellbeing influences our choices, whether adopting healthy lifestyles or managing long-term conditions. Our outlook also influences how well we take advantage of social and economic opportunities. Positive wellbeing fosters confidence which in turn feeds a virtuous cycle. Negative wellbeing saps our energy to deal with the stresses of life. This can lead to a vicious cycle where stresses knock our confidence and undermine our resilience, leading to more stress as we fail to cope. This complex interplay may help explain how individuals deal with everyday issues from navigating health care to managing work-life balance and why some thrive while others languish in the face of apparently similar challenges.
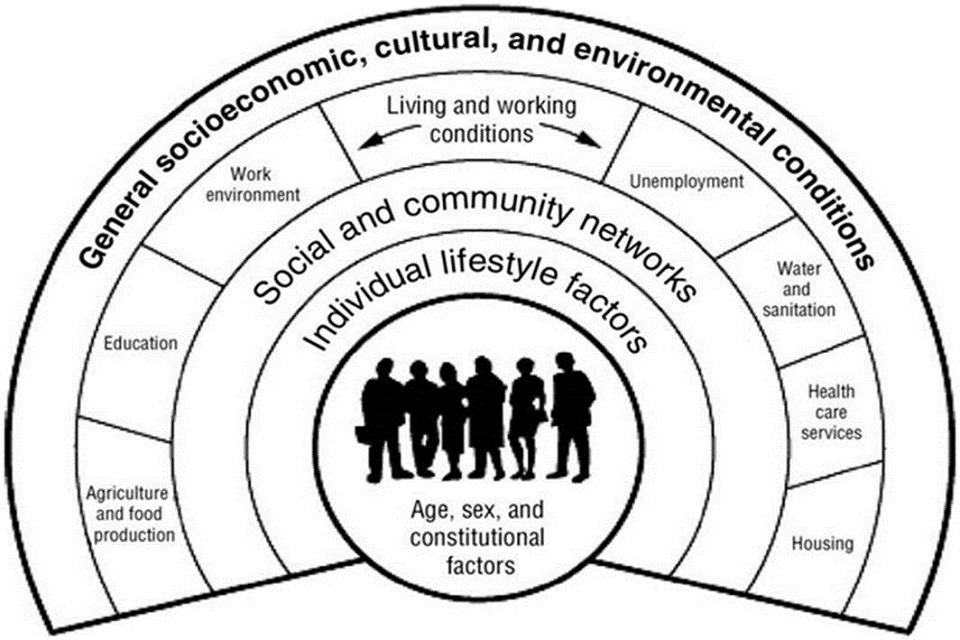
At an individual level it is important not only to prevent mental ill health but to promote positive wellbeing. This will only be successful if we recognise that our mental health is influenced by our physical health, our socioeconomic status and the quality of our relationships. Some factors are in our control but many are not. It is the factors that are not within our individual control that are the focus of public health action. Poverty is not good for mental health. A simplistic view would be to encourage the individual in poverty to work harder or smarter to overcome their situation but what if the odds are stacked against you? What if the outcome depends more on where you start in the socio-economic sweepstakes than on the effort you make? It is well documented that income inequality strongly correlates with poorer population health outcomes including measures of mental health.
The COVID-19 pandemic and the national lockdowns were a shared experience, but the context for that experience varied widely. Much of that context was in place before COVID-19 and will persist if deliberate action is not taken. We need to foster social and economic conditions that help people to thrive but we also have to work with people whose outlook has been shaped by adversity and low expectations that make it difficult for them to see new opportunities that arise. This report aims to inform the conversation about how we help our population and our communities to be resilient in the face of COVID-19 impacts and to create conditions where everyone can thrive.
Understanding the challenge
The national picture
Annual surveys have found that in any given year, one in six adults will experience a common mental health problem and mental health problems are the second leading cause of ill health in England. Half of all mental health problems have been established by the age of 14, rising to 75% by age 24 [1]. Emotional and mental wellbeing are significantly shaped by the social determinants of health into which we are born, live, learn and grow.
Mental health problems are unevenly distributed across society with disproportionate impacts on people living in poverty, those who are unemployed and vulnerable population groups including sexual and gender minority groups and Black and Asian minority ethnic groups.
The life expectancy of someone with a serious mental health problem is 15 to 20 years lower than the general population. Two thirds of these deaths are from avoidable physical illnesses, including heart disease and cancers.
In England, someone with a serious mental illness under 75 is:
- Almost 2 times more likely to die from Cancer
- Over 3 times more likely to die from Cardiovascular Disease
- Almost 5 times more likely to die from Liver or Respiratory Disease [2]
Mental health problems represent the largest single cause of disability in the UK. Before the pandemic, the cost to the economy was estimated at £105 billion a year [3], roughly the cost of the entire NHS. Perinatal mental health problems alone carry a total economic and social long-term cost to society of about £8.1 billion a year.
People with long term physical illnesses suffer more complications if they also develop mental health problems, increasing the cost of care by an average of 45%. People with high levels of wellbeing are more likely to recover and survive from an illness than those with low baseline levels of wellbeing. Among 15 to 17 year-olds, higher levels of wellbeing are associated with a lower likelihood of engaging in health risk behaviours, such as smoking, risky sexual behaviour or drug use.
The local picture
With a population of over 136,000, Torbay is the second largest urban area within the South West. Not only a popular tourist destination, Torbay is also a retirement destination for many fit, active, skilled and affluent older people which is reflected in the population structure.
Like many coastal areas, Torbay faces big challenges. There are high levels of poverty and deprivation, with not enough opportunities for young people. Torbay currently has a predominantly low-wage, low-skill economy and a heavy reliance on the tourism industry on which the COVID-19 pandemic has had a significant impact [4].
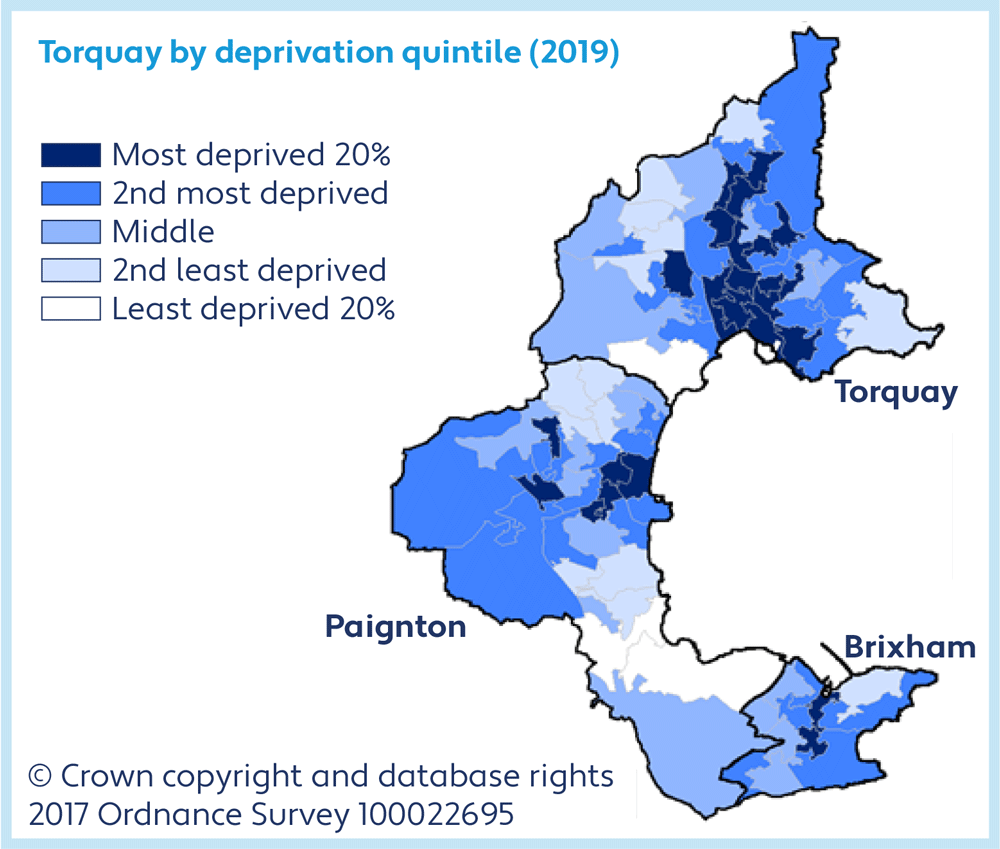
Torbay was ranked as the 38th most deprived upper-tier local authority in the 2019 Index of Multiple Deprivation and the most deprived in the South West. These figures, along with the knowledge that emotional and mental wellbeing are influenced by poverty, unemployment, drug and alcohol use and by the life into which someone is born, highlight the challenges facing the mental health of Torbay’s population.
| Area | Aged under 18 | Aged 18 to 64 | Aged 65 and over |
|---|---|---|---|
| Torbay | 25,484 (19%) | 73,591 (54%) | 37,143 (27%) |
| England | 21% | 60% | 19% |
Out of 100 in Torbay
4 out of 100 school pupils are identified with a primary special educational need of social, emotional and mental health (2021)
18 out of 100 children under 16 are in relative poverty (2019/20)
3 out of 100 children under 18 have been identified as ‘in need’ due to abuse or neglect (March 2021)
5 out of 100 are not in education, employment or training (2021)
18 in every 100 aged 16 and over are estimated to have depression or anxiety (2017)
4 in every 100 16 to 64 year-olds are receiving Employment Support Allowance for mental and behavioural disorders (November 2020)
14 out of 100 adults have an unresolved diagnosis of depression on their GP record (2020/21)
24 out of 100 of those with a long-term mental health condition smoke (2019/20)
31 out of 100 adults are physically inactive (2019/20)
68 out of 100 adult carers do not have as much social contact as they would like (2018/19)
65 out of 100 adult social care users do not have as much social contact as they would like (2020/21)
12 out of 100 aged 65 and over are estimated to have depression or anxiety (2017)
17 out of 100 adult social care users aged 65 and over feel they have no control over their daily lives (2020/21)
Deprivation has an impact on alcohol specific conditions across the population. Torbay has significantly higher rates for ‘alcohol related hospital admissions’ for both the 40-64 population and the under 18s compared both nationally and regionally. ‘Alcohol specific hospital admissions’, also high, are those that are solely relating to alcohol.
| Area | 40 to 64 | 65+ |
|---|---|---|
| Torbay | 1240.0 | 1044.5 |
| England | 887.4 | 1030.4 |
| Area | 2013/14 - 15/16 | 2014/15 - 16/17 | 2015/16 - 17/18 | 2016/17 - 18/19 | 2017/18 - 19/20 |
|---|---|---|---|---|---|
| Torbay | 67.8 | 54.2 | 60.5 | 78.7 | 72.0 |
| South West region | 46.8 | 44.4 | 43.6 | 44.1 | 45.4 |
| England | 37.4 | 34.2 | 32.9 | 31.6 | 30.7 |
Mental health inequalities are a real challenge for Torbay. People living in the area are more likely to experience poorer mental health outcomes compared with those living in other parts of the region or country.
Suicide is a significant cause of death in young adults across the UK. In Torbay, suicide rates amongst young adults are consistently higher compared both regionally and nationally and are an indication of wider mental health issues amongst the local population.
Suicide rate per 100,000 2018-2020 (age standardised)
- Torbay - 18.8
- England - 10.4
| Area | 2010 - 12 | 2011 - 13 | 2012 - 14 | 2013 - 15 | 2014 - 16 | 2015 - 17 | 2016 - 18 | 2017 - 19 |
|---|---|---|---|---|---|---|---|---|
| Torbay | 10.3 | 13.0 | 13.6 | 13.1 | 14.0 | 15.7 | 19.5 | 19.0 |
| South West region | 10.9 | 11.3 | 11.3 | 11.0 | 10.8 | 10.6 | 11.1 | 11.3 |
| England | 9.5 | 9.8 | 10.0 | 10.1 | 9.9 | 9.6 | 9.6 | 10.1 |
Emergency self-harm admissions have fallen over the last few years in Torbay but they remain significantly higher than the England average for both females and males.
| Sex | 2016/17 | 2017/18 | 2018/19 | 2019/20 |
|---|---|---|---|---|
| Female | 187 | 166 | 152 | 140 |
| Male | 100 | 99 | 91 | 85 |
Hospital admissions relating to self-harm amongst 10 to 24 year olds in Torbay are significantly higher than regional and national rates.
| Area | 2013/14 | 2014/15 | 2015/16 | 2016/17 | 2017/18 | 2018/19 | 2019/20 |
|---|---|---|---|---|---|---|---|
| Torbay | 563.9 | 921.0 | 1160.5 | 877.8 | 949.2 | 784.6 | 700.7 |
| South West region | 521.2 | 538.2 | 598.1 | 582.0 | 621.0 | 679.3 | 659.9 |
| England | 415.8 | 401.9 | 430.5 | 407.1 | 421.2 | 444.0 | 439.2 |
Failure to treat mental health disorders in children can have a serious impact on their future, resulting in reduced job and life expectations.
Hospital admission rates relating to mental health within Torbay for girls under 18 have been significantly higher than the England average since 2013/14.
| Ages | Female | Males |
|---|---|---|
| Under 18 | 72% | 28% |
| All ages | 51% | 49% |

Many mental health conditions are preventable and almost all are treatable, so people can fully recover or manage their conditions successfully and live healthy, happy and productive lives. Without question, the COVID-19 pandemic has had an impact on the mental health of many. Good mental health supports good physical health and is key if we are to self-care for long term conditions, support our children, and our community, as well as engage in a lifestyle that encourages us to live well.
Catherine Lissett, Consultant in Diabetes and Endocrinology and System Medical Director, Torbay and South Devon NHS Foundation Trust
The picture post-pandemic
The COVID-19 pandemic and lockdown response has been preventative and protective for some population groups, while intensifying risk factors and vulnerabilities for others. Mental health and wellbeing worsened during the first national lockdown and access to services, including hospital referrals and GP appointments, decreased by 61%. Of those who tried to access NHS mental health services, 25% were unable to get support. A further one in three adults, and more than one in four young people, did not try to access support during lockdown because they did not think that their problem was serious enough[5].
Some groups are particularly likely to have experienced mental health impacts from the pandemic:
- People with existing mental health issues
- Young women
- School age and young people
- People with learning difficulties
- Black, Asian and minority ethnic population groups
- Sexual minority groups (LGBTQ+)
- People experiencing financial insecurity
- Health and social care professionals.
A Public Health England study found evidence of an increase in anxiety and low wellbeing during the first national lockdown. The findings suggest that depressive symptoms had a greater impact on young people and on women. It also indicated that the experience of depression amongst those with financial vulnerability had risen from 21.1% before the pandemic to 34.9% in June 2020[6].
The pandemic has had a significant impact on Torbay. Existing deprivation and social inequalities have widened over the last two years. An ageing population with many people drawn to Torbay for retirement and over half of residents over the age of 50, has led to significant increases in loneliness and inactivity. The hospitality and tourism industry suffered dramatically through the periods of lockdown, leading to job losses and reports of food insecurity. Torbay’s support services saw immediate and substantial increases in people reaching out for help, including those who had never been in crisis before, and agencies continue to face unprecedented pressures. We need to overcome these challenges by responding as a whole system to support our most vulnerable residents.
Starting well
Torbay is home to around 27,784 children. As a system, our objective is to ensure that each one of these children not only gets the best start in life, but also is supported to make positive choices that influence their future.
We know that emotional wellbeing and resilience has its foundation in our earliest experiences, with evidence that the first 1001 days, beginning in pregnancy, is a significant and influential phase in development. The Nurturing Care Framework, published by UNICEF, the World Bank and the World Health Organisation states:
Investing in this period is one of the most efficient and effective ways to help eliminate extreme poverty and inequality, boost shared prosperity, and create the human capital needed for economies to diversify and grow[7].
Ensuring every child gets the best start in life is a critical challenge challenged in the context of high rates of domestic abuse and substance misuse, increasing numbers of people living in poverty and significant numbers of those living with mental illness.
Torbay is home to 25,423 children
21 out of 100 children are part of a low income family
58 out of 100 infants are not breastfed at 6-8 weeks
29 out of 100 children are not 'school ready' by the end of reception. For those children eligible for free school meals this rises to 47 out of 100
25 out of 100 reception aged children are overweight or obese. By Year 6 this rises to 35 out of 100
There are 51 pregnancies to women aged under 18
36 out of 100 school children are not physically active or fairly active
13 out of 100 babies are born to mothers who were smokers at the time of delivery
18 out of 100 children have Special Educational Needs
6 out of 100 16 and 17 year olds are not in education, employment or training
35 out of 100 children aged 5 have one or more decayed or filled teeth
44 out of 100 admissions for self-harm relate to 10 to 24 year olds
There were 1,220 births during 2018
There were 821 recorded occurrences of domestic abuse where children were present during 2018/19
The challenge we face
In Torbay there are 320 cared for children, 179 children subject to Child Protection Plans and 1067 children in need[8]. Improving outcomes for these children and their families remains a key issue for Torbay, system wide. These numbers represent the ongoing challenge of ensuring all our children and young people are safe, happy and healthy so they can reach their full potential. We are committed to improving outcomes for these children, young people and families, and reducing the numbers of children needing child protection interventions.
Self-harm remains a key priority for agencies and individuals supporting children and young people in Torbay. We know children turn to self-harm as a mechanism to manage distressing and overwhelming life experiences and thoughts. In Torbay, almost half of all hospital admissions relating to self-harm are in young people aged between 10-24 and rates are continuously higher compared both regionally and nationally. No child should resort to self-harm to help them cope with life stressors, and it is our collective ambition to significantly reduce these alarming numbers whilst providing rapid interventions for the children and families affected.
The COVID-19 pandemic created increasingly complex issues for Torbay’s children, young people and families. Interventions to help contain the disease - including online learning and pausing of face to face mental health support - have had a negative effect on mental health and wellbeing. Psychological distress, anxiety and depressive symptoms appeared to peak in April 2020 and although there is evidence of some recovery since that time, we are not yet back to prepandemic levels.
COVID-19 has had a disproportionate impact on children and young people who experienced existing inequalities. For the 821 recorded occurrences of domestic abuse where children were present in 2019, these children would potentially have been exposed to further abuse as stresses on families intensified and the gap in interventions grew. Those already experiencing abuse or neglect by household members were subjected to prolonged exposure to potential harm.
The pandemic has highlighted digital exclusion and considerable divides between those able to access technology across Torbay, with the poorest families being the most significantly affected. Vulnerable children and young people have faced reduced access to education and support, whilst online support for people with Special Educational Needs was difficult to achieve. Midwifery and health visiting services were moved online, with missed opportunities to safeguard vulnerable children and families. People unable to access the digital world are often unable to access support.
75% of respondents agreed that they found the second lockdown harder to cope with
than the previous, including 44% who said it was much harder. Young Minds
In 2020, Kooth handled proportionally 51% more service users presenting with eating disorders in comparison to 2019, and 103% more than in 2018.
Paediatrics reported a three-to-four-fold increase in referrals for eating disorders since the start of the pandemic. RCPH, 2020
67% believed that the pandemic will have long term negative effects on their mental health. Lost Generation.
Suicidal thoughts are up 54% for the 10-13 age group. Young Minds
2020/21 - sleep difficulties up 98% in Kooth users and in University attenders up 161%.
Loss of aspiration and motivation up 115% in Kooth users 2020-2021.
10-13 year old service users presenting with self-harm issues were up 33% in 2020 compared to previous year. Kooth
63% of CYP presented in the ‘severe’ category on CORE. This varied throughout the year with noticeable spikes in April and December 2020, coinciding with the first and second lockdowns. Kooth.
The pandemic hit the poorest children in Torbay hardest, especially those from Black, Asian or other Minority Ethnic backgrounds. A disruption to support services meant refugee and migrant children and young people, young carers and those with additional needs have been significantly affected.
How the pandemic has affected our children and young people
- more children are saying they feel lonely and isolated
- problems with anger
- increase in risk behaviours
- low self-esteem
- high numbers reporting depression and anxiety
- more young people reporting self-harm and suicidal thoughts
- problems coping with school and friendships
- more children appear withdrawn and anxious
It is important to highlight the challenges facing children and young people in need of specialist mental health support, and the resource strains facing statutory mental health provision. Increasing numbers of children and young people need assessments and help, a trend exacerbated by the pandemic.
Children and young people can be waiting a long time for specialist assessment, or not meet the threshold for specialist care. Torbay’s agencies and interventions for young people go some way towards bridging the gap, but we cannot ignore the significant challenge for the collective system in promoting and protecting the mental health of our vulnerable children and young people.
There is a programme of investment in specialist services alongside a trajectory for improvement.
A key priority continues to be to support individuals who have low-level mental health needs, recognise the life stressors that can lead to a mental health crisis, intervene before a statutory referral is needed. Increasing attention must be on ensuring people can access the help they need, at the time they need it, and at the appropriate level.
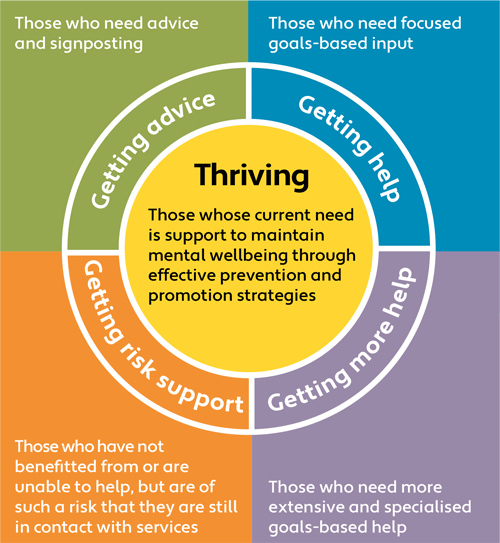
THRIVE is an integrated approach to delivering mental health services for children, young people and families. It is person-centred and needs-led and conceptualises need in five categories:
- Thriving
- Getting Advice
- Getting Help
- Getting More Help, and
- Getting Risk Support[9].
Trauma informed
The trauma informed vison sits as a core set of principles within strategy, policy and procedure across the wider Torbay partnership. It provides a framework for preventative working. We work with the Substance Abuse and Mental Health Services Administration definition of the trauma-informed programme, organisation, or system, which:
- Realises the widespread impact of trauma and understands potential paths for recovery
- Recognises the signs and symptoms of trauma in clients, families, staff, and others involved with the system
- Responds by fully integrating knowledge about trauma into policies, procedures, and practices
- Seeks actively to resist re-traumatisation [10]
What we are doing in Torbay
Torbay has a wealth of dynamic statutory, voluntary and community services that collectively have a clear and consistent vision for children and young people.
Torbay’s 2018 - 2023 Children and Young People’s Plan, updated in February 2021 as a response to the changing needs due to the pandemic, has been written by a range of partners, including young people themselves. The plan draws upon the evidence base provided by both our Joint Strategic Needs Assessment (a picture of the needs of our communities) and Torbay’s Sufficiency Strategy (setting out out the council’s clear intention to significantly improve the way in which we provide services to children who are cared for or are on the edge of care). The plan is intended as an overarching strategy for all services which have a direct impact on Torbay’s children and young people.
Priorities include:
- Children get the best start in life
- The impact on children and families from domestic abuse, alcohol and substance misuse and all forms of child exploitation is reduced
- Education outcomes for all children and young people are improved
- Young people are healthy, make positive choices and influence their own future
In Torbay, the council’s commissioning programme delivering the 0-19 service is already in Year 3 of operation. This integrated service brings together Health Visiting, School Nursing, Children’s Centres and specialist Children’s services. It is a nine-year programme (2019 –2028) focussed on dynamic, flexible services working in partnership with communities, with early help as its focus.
With a range of family hubs in children’s centres, there have been significant investments in digital improvement. Online parent/carer support through Parent Talk and online child development courses are available to all Torbay residents covering a wide range of developmental learning, from antenatal to the teenage brain. [11] [12]
Torbay’s mental health support teams provide opportunities for support for children and young people with emerging, mild or moderate mental health difficulties which have an impact on day-to-day life. Interventions can be accessed by children and young people, parents and carers. Support is also offered directly to school leadership teams to help them identify mental health need within their school community and develop strategies that support a whole school approach to mental health [13].
The Devon Self Harm Service is led by the Children’s Society in Torbay and is a two-year pilot aiming to provide early interventions to support young people age 11 to 18 who are selfharming. The service is informed by a combination of Cognitive Behavioural Therapy (CBT), Dialectal Behavioural Therapy (DBT) and Mentalisation based approaches. One to one and group work sessions are offered to young people. The service also provides support to school staff, contributing to assessments of young people, raising awareness, sharing resources. Through the pandemic, a revised service offer using video conferencing, SMS telephone support and some limited face to face support was put in place [14].
knowledge and providing

At South Devon College we believe that emotional wellbeing in our students is as important as academic outcomes. Teaching students about good mental health and personal wellbeing provides them with the tools and strategies needed for building their resilience to deal with whatever life throws at them.
Our three top priorities are:
- Making mental health support and personal wellbeing available to every student
- Teaching our learners and training our staff in mental health education so they know how to recognise mental health related issues in themselves and others, and how to access support so that we can improve lives and save lives
- Listening to our students and acting quickly when things go wrong for them.
Laurence Frewin, Principal and CEO, South Devon College
Kooth.com
Kooth is a free, safe, confidential, and non-stigmatising way for young people aged 11-18 to receive counselling, advice and support online. Kooth delivers thousands of counselling sessions each year across the UK with counsellors available until 10pm each night, 365 days a year, providing much-needed out of hours advice and help.
CheckPoint, The Children’s Society
CheckPoint provides help to young people aged 8-18 on the phone, online and face-to-face. It offers young people support to overcome challenges that are holding them back, to help them achieve the things that matter to them, and to provide skills and strategies to deal with problems. Everyone needs a helping hand from time to time; Checkpoint helps hundreds of children and young people with specific mental health challenges every year.
Torbay Wellbeing Service
Torbay Wellbeing Service is a partnership between 0 to 19 Torbay, CheckPoint, South West Family Values, Young Devon and Imagine This. It provides services designed to help children and young people with practical issues, offering:
- Wellbeing conversations with a therapist focusing on how things are for the young person and the things they are struggling with
- Wellbeing drop-ins where a young person with something on their mind can attend without an appointment and speak to someone
- Individual cognitive behavioural therapy with Wellbeing Practitioners to help children and young people understand the links between what they think and feel and how they act
- A Wellbeing café, a friendly, relaxed place where young people can meet other young people and share ongoing support
- Therapist counselling for young people to talk through the things that matter to them.
Case Study - Jade’s Story
My life before going to The Children’s Society, I wouldn’t even call it a life. I wouldn’t leave the house. I could feel myself getting worse, to the point where I did once try to take my life, but I was too scared to do it. I think I would be dead by now,if it wasn’t for The Children’s Society.
When I first came, I didn’t believe it would help, but I was doubtful of so many things. I was terrified, I was terrified of getting better. And then when I came here I started to think “OK, I think I could get better here.” I could look at myself in the mirror again, or just talk to a new person. And it did help so much. And I can say that I am better now, and I am very proud of what I have done.
Plans for the Future
In 2020, the government Early Years’ Healthy Development Review set out an ambitious transformation programme for supporting families. Our priorities in Torbay are based on these same six action areas:
- Early help for families, building resilience in partnership with families and communities including maternal and pre-conception support
- An accessible range of community and virtual locations for families to support early child development through the first 1001 days. These are the building blocks of future resilience and emotional capacity
- Support for key transitions in a child’s journey and at significant life events
- Workforce development and retention including alliance commissioning with providers
- Investment in data and intelligence and partnership working
- Leadership, supporting the Torbay system to be sustainable and resilient.
Chapter 4 - Living Well
Often when we think about mental health, we consider whether someone has a clinical diagnosis of a mental health condition such as anxiety, depression or bi-polar disorder. But a diagnosis is just a small part of what creates ‘good’ or ‘bad’ mental health. Achieving and maintaining good mental health requires good wellbeing, and this can be determined by the social factors in which someone lives. This is a particular challenge for Torbay, with comparatively high numbers of people living in poverty, high unemployment rates and significant numbers of people with drug and alcohol problems.
The broad social and economic circumstances that together determine the quality of the health of the population are the ‘social determinants of health’.
Collectively and as a system of agencies, communities and individuals striving for better mental health, we are committed to tackling the stigma associated with poor mental health and wellbeing, enabling and empowering individuals within communities to talk about their mental health and to seek the help they want, when they need it. [15]
Case Study - Graham’s Story
Graham is in his early 30s, he lost his job at the beginning of the pandemic and was living with an abusive partner. The abuse was becoming unbearable and one of the few friends that he had, noticed that he was losing a lot of weight. Graham was forced to leave his home and the reality of losing his relationship, being homeless and having no money coming in, really started to bite. Graham had never felt suicidal before but for the first time, it felt like a real possibility.
The challenge we face
Before the pandemic, one in four Torbay residents said they had high anxiety levels and around one in five residents reported having a common mental disorder such as anxiety or depression. A small proportion of the population was supported for severe mental health disorders by their GP and statutory mental health provision. Suicide and selfharm were significant issues for Torbay’s communities.
Since the start of the pandemic, the mental health and wellbeing needs of Torbay’s population has intensified, with people experiencing new symptoms of distress, anxiety and depression. Sleeping problems and disordered eating have become more prevalent. Additionally, people with a mental health diagnosis have found that their condition has worsened, with access to face-to-face support cancelled or transferred online. The pandemic has caused a rise in external stressors for Torbay’s residents, for example job loss, debt, domestic abuse and a lack of social contact, all having an impact on someone’s ability to cope. As a response, those with existing mental health illnesses found their conditions worsened.
The pandemic challenged our ability to meet very basic needs and to nurture the things that make us feel better such as positive social connections and feeling safe in our community. As an example, food insecurity and worklessness caused by the pandemic is associated with increased risk of mental illness. According to a recent BMC study, food insecurity is associated with a 257% higher risk of anxiety and a 253% higher risk of depression. Losing a job during the pandemic is associated with a 32% increase in risk for anxiety and a 27% increase in risk for depression [16]. Nationally, the Trussell Trust reported a 47% increase in people accessing food banks in the six months from March to September 2020 compared with the same period the previous year. The Torbay Food Alliance has provided over 350,000 meals for people in Torbay since March 2020.
A combination of, or just one, life stressor can intensify an individual’s sense of hopelessness and lack of self-worth, making them feel as though they have no way out of the crisis they are in. Even before the pandemic, suicide was a considerable public health issue for Torbay, with rates increasing year on year since 2010. Suicide rates have not increased nationally or locally during the pandemic, however, international research tells us that after a large strain on a country’s economy, suicide rates are likely to rise. Suicide is the leading cause of death for men under 50, young people and new mothers, with people living in poverty affected the most. When we consider the impact of the pandemic on the emotional and mental wellbeing of Torbay, on people’s jobs, relationships and feelings of self-worth, we are collectively faced with a critical challenge to support individuals and families in crisis.
Case Study - Jessica’s Story
Jessica is in her late 50s and was in a tough situation. She had just lost her husband, was getting behind on rent and was soon to be homeless. Jessica rang the Torbay Community Helpline for a food parcel (distributed by partners of Torbay Food Alliance) to get her through the week but she wasn’t in the right place to talk about her mental wellbeing even though she knew she was struggling. The Torbay Community Helpline called her once a week for three weeks to check-in and on the third week she had built up enough trust so felt ready to have some extra support with her mental wellbeing. She was matched with a Specialist Befriender who specialises in grief and bereavement support, and they are in regular contact, supporting her day by day as needed.
Further challenges lie in the service provision available to people in crisis. In Torbay, the increase in the level of need when people are accessing services means there is extra strain on Torbay’s already stretched mental health services. The Centre for Mental Health forecasts that mental health needs will increase substantially with each wave of COVID-19. The current prediction is that 20% of the population will need new or additional mental health support as a direct result of the pandemic. Almost two thirds will already have an existing mental health need (including severe mental illness) with a significant proportion needing support for depression or anxiety or both[17]. In Torbay, this means that around 7,400 will have a new mental health need and 14,800 will have an additional mental health need.
In striving to reduce stigma, mental ill health and suicide rates in Torbay, we must first have a system that is enabled to protect and safeguard individuals before they reach crisis point. People and families affected by mental ill health and suicide by association must also be supported. Protecting individuals and communities from mental ill health and suicide is complex, but collectively we are ambitious in striving towards improved mental and emotional wellbeing for Torbay’s population.

Over the last year, there have been unprecedented demands right across the health and social care system. Our communities faced a challenging future brought sharply into focus by the COVID-19 pandemic. As an Integrated Care Organisation, we are here to support our communities to live well and independently, and to manage their own health and wellbeing as close to home as possible. We know that people’s mental health affects their physical health and vice versa. We are committed to working with our partners to support the whole person and to ensure
parity of esteem across mental and physical health.
Liz Davenport, Chief Executive, Torbay and South Devon NHS Foundation Trust
What we are doing in Torbay
A new partnership model for community mental health is being developed across Torbay and the rest of Devon for people with severe and enduring mental illness. The model offers a clear vision supporting people where they live, with local specialist teams aligned to GP Primary Care Networks working together to provide care and support. As part of this new model, the community and voluntary sector will also target support to tackle loneliness and isolation and digital exclusion, and to bridge the gap between talking therapies and acute support.
Community Mental Health Framework
The wider Devon Integrated care system (ICS) includes the local authority areas of Devon, Torbay and Plymouth and sets out ambitious plans to improve health and transform care services [18]. A key theme is an increased focus on the prevention of mental ill health supported by the publication of Public Health England (now the UK Health Security Agency)’s ‘Concordat for Better Mental Health, 2020’. Partners across Devon, Plymouth and Torbay are committed to working together to improve mental health outcomes and reduce suicides. We have developed a Devon-wide Suicide Prevention Strategic Statement with the objective of working together to make all communities in Devon, Plymouth and Torbay suicide safer communities.
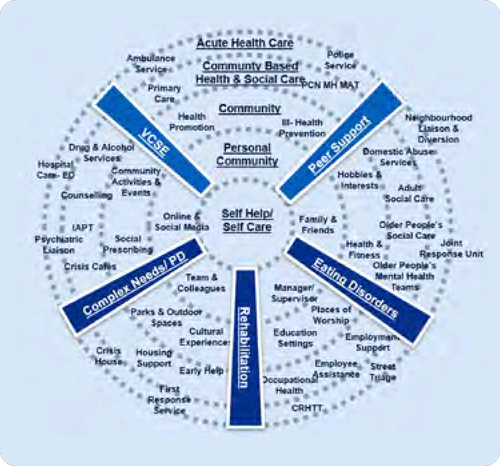
Self Care
At the centre of our core model is the person and their capacity to care for and help themselves.
Personal Community
when a person has a problem, the first people they turn to are those in their personal network - their family, friends, colleagues and online network.
Community
People exist in communities, a person’s community will include the people and places where they contact others, at the school gate, in their place of work, through community events, hobbies and interests.
Community Based Health and Social Care
Within communities, but not often part of our daily lives, is a range of community based health and social care support which aims to help us when we are unwell.
Acute Health Care
Within our wider communities, we have a more specialist range of health, social care and other community services, which help us when our needs are more urgent and acute.
Building on the successful partnership working of a small, reactive and dynamic Mental Health Cell initiated at the beginning of the pandemic, the Torbay Mental Health and Suicide Prevention Alliance was formed in September 2020. This alliance is made up of public bodies including Torbay Council, statutory mental health services, the police, Torbay Healthwatch, Torbay Primary Care Networks and community voluntary sector partners such as Torbay Community Development Trust, Age UK Torbay, Action for Children and Action to Prevent Suicide.
These agencies collaborate with the aim of improving mental health outcomes for Torbay’s population, improving access to the right support at the right time, and preventing and reducing the impact of suicide on the community. This is achieved through:
- Promoting early identification and rapid response
- Identifying gaps in provision
- Mapping local resources supporting mental wellbeing
- Promoting clear pathways of support across the continuum of mental health
- Ensuring a trained, supported and informed workforce
- Developing consistent messages across organisations concerning the importance of mental health
- Sharing resources and promoting community collaboration
- Developing learning, good practice, knowledge and skills
- Seeking out opportunities to promote mental wellbeing across Torbay
Torbay’s sense of community can be reflected in the rich and diverse services available to people in need of mental health and wellbeing support. These creative initiatives have a positive and lasting impact on the community, amplifying Torbay’s great sense of togetherness.

Torbay Community Helpline
The helpline is one of the true success stories of this pandemic. Initially launched as the Torbay Community Coronavirus Helpline back in March 2020, one week before the first lockdown, it has taken more than 25,750 calls – each one of those from someone who needed help.
The helpline has grown from providing food and medication support to those who had to self-isolate, into a multidisciplinary support service dealing with everything from mental health to telephone befriending, financial support to domestic abuse support.
Case Study - Torbay Community Helpline
David Gledhill, Torbay Community Development Trust
In total, staff of numerous charities in the Bay led by the Torbay Community Development Trust, AgeUK Torbay, Brixham Does Care, Healthwatch Torbay and Citizens Advice Torbay have worked alongside an army of volunteers to help and support more than 4000 people.
We have provided information and advice to people who, very often, had nowhere to turn when the world began to change; the roads fell silent, the doorbell stopped ringing and they were forced into self-isolation.
At first, not everyone had the support of friends, neighbours or relatives to go shopping or pick up their prescriptions. Some didn’t even have anyone to talk to and went for weeks at a time in relative silence.
Our Rapid Response Team went shopping, collected prescriptions, provided befriending and a helping hand.
Before the crisis started, we estimated there to be 6000 lonely and potentially isolated people in the Bay out of a population of 135,000. We now believe there to be thousands more.
In the last 18 months everything that we recognised as our normal everyday life has been turned on its head. This has had a significant impact on us all and particularly in relation to our mental and physical health and wellbeing.
People felt they had become imprisoned in their homes too afraid to go out and fearing that they would never go out again or see family and friends. People cried at the thought of never hugging family members or holding their hands. People lost jobs, financial security, faith, roles and responsibilities, friendships, loved ones and a sense of value or worth.
The practical and emotional challenges of poverty, debt, homelessness, hunger, abuse, fear, isolation and loneliness have increased.
The challenges that people had to cope with prepandemic were for many increased dramatically during the last 18 months and have created the need or continuing mental health support both at the present time and in the future.
Jane Eastwood, Torbay Community Helpline Manager, Mental Health
Workplace wellbeing
Employers play an important role in supporting the mental health and wellbeing of residents, particularly when many of us spend most of our week at work. Fulfilling employment has a positive impact on our sense of worth. If employees feel their mental health and wellbeing is supported by their employer, this has a positive impact on both the workforce and the business.
Research has shown that staff who have good mental health and wellbeing and feel supported with their mental health conditions are more productive and jobs are retained. In 2021, Torbay Council appointed our Director of Public Health to be a ‘Council Wellbeing Guardian’ alongside other key figures in our community. This means that he will provide oversight, assurance and support to the Council’s senior leadership team to promote the health and wellbeing of Council staff. This strategic focus aims to bring about real cultural change across Torbay Council and give traction to some great initiatives that are already in place:
- Growing Wellbeing Supporters – Torbay Council employees who have been trained to spot the signs of poor wellbeing in staff and have supportive conversations
- Staff counselling service – to support staff when they need it
- Intranet pages that give self-help information on improving wellbeing
Many of Torbay’s businesses and employers are investing in staff wellbeing in similar ways. Collectively our ambition is to continue to build wellbeing networks to share best practice across the Bay.

For any business, staff form the most precious resource. The wellbeing and mental health of those employees and indeed the owners and managers themselves form a fundamental pillar for a sustainable business.
Ensuring that the workforce is both happy and at work, with a good balance of life and meaningful employment, is paramount when seeking to achieve sustainable business growth.
A stable business landscape is vital to help provide security and confidence and to steer us away from the emotional rollercoaster that we have all been riding through COVID-19.
Steven Reynolds, Chair of Torbay Business Forum
Case Study - Brixham Bee Well
Before the pandemic, a group of people who live in Brixham felt they wanted to do something positive to help people in their town. Brixham is a close-knit community and a beautiful place.
Brixham Bee Well wanted to build on these assets by offering a safe space and a listening ear to all welcome local residents and businesses who would like to be part of some positive action to support their community. This might include getting free training on how to have open conversations about mental health and wellbeing or offering their business – shop, café, hairdressers or taxi company - as a safe welcoming place for people when they are struggling with their wellbeing.
Plans for the Future
The Torbay Suicide and Self-harm Prevention Plan 2021-22 has six priorities for action:
- Reducing social isolation and loneliness
- Promoting a ‘culture of curiosity’ both publicly and professionally
- Building upon and growing peer-support within the mental health system
- Better understanding Torbay’s high suicide and self-harm rates
- Addressing system gaps for people with severe mental illness (in partnership with the Community Mental Health Framework redesign)
- Tackling high frequency suicide locations
Torbay’s grassroots community initiatives continue to be supported and resourced with the aim of preventing suicide. This is achieved by raising awareness, training primary care staff and others in frontline roles in suicide prevention, researching into suicide and self-harm in Torbay, and promoting Samaritans’ guidelines on media reporting. Next year Torbay will have:
- Trained local trainers to deliver Community Suicide Awareness and Resilience courses which can be safely delivered online (something that has proven essential during the pandemic).
- Provided free Community Suicide Awareness and Resilience courses to the public and professionals who are likely to meet people who are at risk of suicide
- Set up a Torbay community grant pot for local suicide prevention projects
- Provided research on people with lived experience of self-harm to better understand self-harm in Torbay from an individual and professional perspective, highlighting the gaps in service provision.
Torbay Wellbeing Engagement Programme
In May 2021, Torbay’s Local Authority Public Health team were awarded funding from the Public Health England Prevention and Promotion Fund for Better Mental Health to address the mental health needs of Torbay’s population post-pandemic. The Project has recruited a team of Wellbeing Coordinators who will work across food banks and children’s centres in Torbay, addressing and preventing mental ill health. Needs may include food poverty, unemployment, housing problems, financial instability and coping behaviours as well as lower-level mental health needs. Support will include the formation of a trusted relationship, supportive conversations, and support to access social or peer support. This project will be fully established over the next year.
An online mental health support platform is being commissioned jointly across Devon, Plymouth and Torbay Public Health teams and NHS Devon. This will offer 24/7 support for adults with mental health issues complementing the KOOTH online platform already in place for children and young people.
Ageing well
Tackling poor mental health and wellbeing requires an approach that takes account of the whole person and their social context. Aspects such as belonging, identity, social connection and purpose are central, as is the environment in which people live. To achieve high levels of mental wellbeing we rely on developing community assets, local relationships and social capital [19].
The challenge we face
There are particular challenges to our mental health and wellbeing as we age, and Torbay has proportionately more older people compared with the England average. By 2030, those living past the age of 75 is expected to increase by 21.9%[20]. The increase in the 75 and over age groups will increase demand for physical and mental health and care.
Torbay Public Health carried out a suicide audit in 2019/20. This involves reviewing coroner’s files to identify the themes and risk factors for people who have sadly taken their own lives. Each case is individual, but there are some shared themes. For those in later life, these include:
- recent bereavement, especially after having cared for a loved one in poor health for many years
- deteriorating illness and fears of being without help and support
- loneliness and isolation.
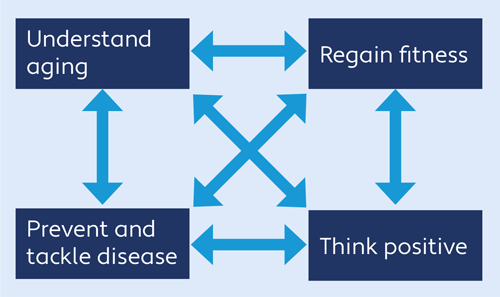
COVID-19 has had an impact on all ages in different ways. For older members of the community, it has led to enforced inactivity and a loss of physical fitness, increased social isolation and separation from family and friends, and fears of going out again for work, hobbies, shopping or socialising. There is a big health and wellbeing deficit as a result of the pandemic which we now need to recover.
Many people retire to Torbay for the beautiful coastal environment, often having visited for holidays in earlier years. If they have no family or social networks in the area, and develop health conditions that restrict mobility, they become more and more socially isolated.
Mental health is both a determinant and a consequence of physical health. Evidence shows that all of the Five Ways to Wellbeing – Connect, Learn, Be Active, Take Notice, and Grow - contribute to positive mental health. ‘Activity therapy’ can help people to manage long-term health conditions and to improve emotional health and resilience. We have traditionally treated physical and mental health in isolation, with different services providing different aspects of care and support. Connecting physical and emotional support is especially important as we age. In ensuring the best health and wellbeing outcomes for Torbay’s ageing population, we acknowledge the system requires a more holistic approach, tackling physical and mental wellbeing together.
What are we doing in Torbay?
Through a better understanding of ageing and the interaction of physical, cognitive and mental health, we want to challenge the inevitability of frailty and decline. Torbay is implementing the Optimal Ageing – Live Longer Better programme which looks to support people to lead lives that are full and rewarding for as long as possible, active, independent and socially engaged.
This also involves changing the language. Rather than talking in terms of ‘caring’, we think of supporting or ‘coaching’, introducing positive concepts such as ‘planning with purpose’ and seeing the onset of a new decade or longterm condition as the time to work on increasing physical activity levels and take up new social activities rather than the opposite. These concepts apply equally to care at the end of life – there are always opportunities to support people to live their last months in the best way possible, doing the things they are able to enjoy, with those they want to be with.
Ageing Well Torbay
Ageing Well Torbay is a seven year project funded through the National Lottery Community Fund which aims to reconnect communities and reduce social isolation experienced by people aged over 50 living in Torbay. Community Builders work in local neighbourhoods encouraging people to get involved in social activities, supporting inclusion, befriending and mental wellbeing. Wellbeing Torbay is delivered by Age UK and Brixham Does Care. Wellbeing Coordinators help people to be active in managing their own wellbeing, health and care.
Case Study - George’s Story
George is 65 and lives in Brixham. George suffers from asthma, osteoporosis and dyslexia which made it difficult to get back into full time employment. He also has a history of alcohol and drug use.
George was linked to an Ageing Well Community Builder who suggested he consider volunteering as something to do with his time. He decided to go to a local charity and worked for their furniture store for two years.
During the winter, George was frequently in touch with his Community Builder as he had hit quite a low point and was experiencing difficulties with his housing. George’s Community Builder provided some practical support with housing, and also encouraged him to get up and out of his flat.
George really enjoyed the activities that he took part in at ‘The Edge’ in Brixham. Without his Community Builder, he would not have participated. She made a big difference to him at the time when he needed it.

During Lockdown many of our older residents were more isolated and lonelier due to shielding and staying in. Digital provision helped, but social lives were suspended, and we know that physical and mental health are closely connected. It will take a long time for people to get back to the way they were, build back confidence, access activities, meet their friends, and get advice and information. Our message is: “Stay Busy, Stay Connected and Stay Active.
It is so important that older people have social activities and hobbies to keep them interested in life, stay independent, and keep them as physically and mentally fit as possible. Sarah
The pandemic and subsequent lock-downs destroyed in many cases the unofficial support networks for the elderly and less able. It will take a long time to restore confidence to get back to a new ‘normal’ but we must all do our best to assist. June
Living with multiple medical conditions is demanding enough, but when your mental health is poor, managing your physical health becomes extra difficult. Without good mental health, your physical health is at risk. Paul
Torbay Assembly
Torbay Assembly
Torbay Assembly has grown from Ageing Well Torbay and provides a forum for people to share views with peers and to advocate for changes to improve the Bay. The Assembly has achieved World Health Organisation Age-Friendly status for the Bay and developed the Torbay Charter promoting age-friendly policies in statutory organisations including Torbay Council. The Assembly is an important partner member of the Torbay Health and Wellbeing Board.
Case Study - Malcolm’s Story
Malcolm is originally from Whitley Bay in the North East, where he lived for nearly 40 years before moving to Torquay 11 years ago. Malcolm doesn’t have any family in the Torquay area. After many years of life pressures including relationship breakdowns and job losses, Malcolm developed anxiety and depression.
Malcolm's doctor directed him to the Depression and Anxiety Services. His counsellor gave him a leaflet about the Community Builders, and eventually, Malcolm plucked up the courage to call. Malcolm’s Community Builder wanted to find out about his interests, hobbies and what he enjoys. As he got to know Malcolm better, he introduced him to other people and asked if he would like to do some voluntary work for the community bus.
Malcolm started volunteering for the community bus once a week, and through this volunteering experience, he met more people.
Malcolm reported that though he still had down times he always had something to look forward to and felt part of his community.
Case Study - Susan’s Story
Susan is 64 and was born in Brixham. She was married for 37 years. After her relationship broke down, her life fell to pieces. She lost her marital home, her children were living elsewhere, and she became unwell.
A Community Builder got in touch with her, and Susan followed their suggestion to enrol in yoga classes at the Edge. She found the atmosphere there to be very relaxed and nonjudgmental, which was just what she needed.
She has found that being able to drop into the Edge, whether for a yoga class or just for a cup of tea, has been a great help. She has met people of all ages, but with a similar outlook. Brixham feels like her safety net, and that is where she has her support network.
More recently, Susan completed a course on Mental Health First Aid and is hoping to get involved in providing support to others experiencing mental health challenges.
Torbay and South Devon Frailty and Healthy Ageing Partnership
The partnership is working across the pathway from identification of frailty to end of life, to improve the health and care experience at each step. Central to this work is supporting the individual as a whole, taking into account both physical and psychological needs, within their family and social context.
Mental wellbeing in care homes
The COVID-19 pandemic has had a substantial impact on the wellbeing of care home residents and staff. Torbay Care Homes Quality Assurance and Improvement Team has been working with care home managers and Devon Partnership Trust to support ‘whole home healing’ as part of post-pandemic recovery. This involves reflecting on their experiences and seeking to build strength and resilience together.
Torbay NHS Foundation Trust is also working on a physical activity project in care homes, which it is anticipated will have a positive impact on residents’ resilience and wellbeing as part of their post-pandemic recovery, working especially with people with dementia.
Partners in Torbay have agreed to implement the Optimal Ageing – Live Longer Better programme. The approach is described above and specific objectives are to:
- prevent and mitigate isolation
- increase physical ability and resilience
- promote knowledge and understanding about living longer better among older people and the wider population to counteract the detrimental effects of ageism
- create an environment in which people can fulfil their potential
- enable strengthening of purpose
- support carers
- minimise and mitigate the effects of deprivation
- reduce the risk of, and delay or prevent dementia
- prevent and minimise the effects of disease and multimorbidity
- enable both living well and dying well
All of these involve or have an impact on mental and emotional health and wellbeing. The programme will be led by the community and bring together and build on the good work already in place across the Bay. As well as practical measures to support individuals to make changes to their lives, the programme seeks to bring about a cultural revolution based on the understanding that people themselves, with the right support, have the ability to improve their own physical, cognitive and emotional wellbeing.
Plans for the Future
Mental wellbeing in care homes
Torbay and South Devon Enhanced Health in Care Homes programme considers mental health as part of the personalised care approach and will be including mental wellbeing in the newly-funded research project looking at the qualitative impact of the framework across local homes.
Carer wellbeing
From the 2011 Census data, approximately one in eight people in Torbay identified themselves as Carers. Actual numbers are likely to be much higher and the 2021 Census is expected to show a far higher figure. Carers UK estimated that unpaid caring increased by 50% during the pandemic, with a significant impact on carer mental health. Torbay Carers surveyed local carers in June 2020 and December 2020 and recorded a deteriorating picture of wellbeing, in particular relating to financial worries. Carers are the foundation of support for our communities and their mental health and wellbeing needs to be a priority.
Mental wellbeing at the end of life
The End of Life Programme is keen to focus on the impact of mental health on advance care planning (planning for the individual’s needs and wishes towards the end of life) and to include mental health more closely with treatment for physical symptoms, as the two are so closely linked. This will also involve greater mental health support for families and informal carers looking after people at the end of their lives.
Management of long-term health conditions
Long-term physical health conditions, and symptoms of increasing frailty, have a major impact on mental health. Partner organisations across Torbay are keen to look at both together and take mental health fully into account when prescribing treatments and care.
Physical activity
Active Devon are building ‘mental health and movement’ into their activity strategy. Torbay Public Health has also developed a project with Active Devon and other partners to promote strength and balance activity for older citizens, working with leisure and activity providers in the Bay. One of the outcomes will be around impact on wellbeing.
We will continue to implement Optimal Ageing – Live Longer Better with partners across the Bay.
Recommendations 2021/22
For all partners across Torbay, supporting the mental health of our staff, clients, patients, students, and communities, is critically important. It is a time of real need, but also a time of real opportunity. COVID-19 has sharpened our understanding of our mental wellbeing. Never has it been more evident that ‘mental health is everyone’s business’. Without good mental health, schools, hospitals, businesses, and communities suffer. With good mental health, we all thrive.
Members of Torbay’s Health and Wellbeing Board have identified mental health and wellbeing as their top priority in the wake of the COVID-19 pandemic. It is also a priority for the new Local Care Partnership covering South Devon and Torbay. This is an excellent basis on which to refocus our efforts to drive improvements in mental health and wellbeing across the Bay.
My recommendations this year build on the innovative work being led by collaborations of voluntary and statutory organisations in Torbay.
Recommendations for 2022
Recommendation 1
Ensure mental health and suicide prevention remain a priority for strategic partners across Torbay.
Recommendation 2
Drive continuous improvement in Children and Young People’s mental health outcomes through a partnership with families and communities.
Recommendation 3
Implement the Torbay suicide and self-harm prevention plan with the aim of stabilising and reducing rates of suicide and self-harm across the Bay.
Recommendation 4
Incorporate mental health and wellbeing into the Multiple Complex Needs alliance from 2022
Recommendation 5
Support the creation of mental health promoting communities through community development, training, safe spaces and peer support.
Recommendation 6
Promote and support workplace wellbeing in all sectors across Torbay.
Recommendation 7
Promote approaches that tackle physical and mental wellbeing together especially physical activity and green spaces to improve wider health and wellbeing.
Recommendation 8
Collaborate with stakeholders to better understand needs and gaps in mental health to inform future planning and quality improvement.
Chapter 7 - Review of 2020/21 Recommendations
In this chapter we review progress against the priorities identified by Dr Caroline Dimond, previous Director of Public Health, in her 2020 annual report.
Recommendation 1
I would like to see a strong focus on work to address health inequalities. Within the council, this is through the Turning the Tide on Poverty work and within the NHS through the Health Inequalities Executive group. This work needs to also take into account the impacts of COVID as evidenced in the latest Marmot review “Building back Fairer” and the analysis on the impacts of COVID that the Public Health team have done. I challenge senior leaders to consider during 2021 how we can bring our efforts on inequalities together utilising this new evidence base to generate a system-wide approach within both the Local Care Partnership and within Torbay’s Primary Care Networks (PCNs) as well as within all council departments.
What have we done
- The Turning the Tide on Poverty programme now underpins Torbay’s COVID-19 recovery strategy and a series of workshops are being held to embed each of the six recommendations of the Marmot review in the recovery workstreams of Torbay Council and partners.
- giving every child the best start in life
- enabling all children, young people and adults to maximise their capabilities and have control over their lives
- creating fair employment and good work for all
- ensuring a healthy standard of living for all
- creating and developing sustainable places and communities
- strengthening the role and impact of ill-health prevention.
- Implementation of the NHS Long Term Plan in the Devon Integrated Care System includes a specific focus on Health Inequalities as a strategic enabler. Local Care Partnerships will
have a key role for delivery as outlined below:
Local Care Partnerships (LCPs) will drive a reduction in health inequalities within their respective areas, eliminating gaps in access to health services for all groups.
By December 2021, LCPs will have developed an understanding of the gaps in access for Black and Minority Ethnic communities, and those living within the bottom 20% deprived areas by Index of Multiple Deprivation. LCPs will, by March 2022, develop plans to show how health inequalities are being considered from the perspectives of access, experience and outcome and will
throughout 2022/23 address barriers to access and any inequity relating to people’s experiences.
Recommendation 2
We need to urgently move the focus to prevention, and in particular, primary preventing looking at behaviours/lifestyle and the determinants of health. Not doing so will continue to burden the health and care sector with increasing demand from preventable illness and also risk lives with any future pandemic.
What have we done
- Worked with the Devonwide Integrated Care System (ICS) to establish the Treating Tobacco Dependence Project over the next three years. This has an acute focus with pathways from maternity, mental health, and hospital inpatients, into stop smoking services commissioned by Public Health
- Delivered the Making Every Contact Count (MECC) Training programme to community and statutory partners
- Evaluated and restructured the Torbay Healthy Learning web-based programme to best meet the needs of education settings as efficiently as possible
- Undertaken a rapid health needs assessment for Lifestyles services to inform our 2022 re-procurement of Lifestyles services in the Bay. This re-procurement will continue to promote and
support prevention activities - Introduced a new Devonwide Child and Young Person’s Weight Management offer, utilising the THRIVE and emerging Early Help Models to create a new approach targeting families most in need
- Delivered the PHE Adult Weight Management Grant with a focus on new 12-week programmes for people with a learning disability in Torbay
- Developed an Oral Health Training Plan for Care Homes and Domiciliary Care to improve oral health residents and clients
- Reintroduced supervised toothbrushing for primary age children and Dental First Steps, increasing access to routine dentistry post-COVID for families with children aged one and above
- Worked with Torbay and Devon Food Partnerships to look at alternative models of delivery in the face of poor uptake of Healthy Start Vouchers and Vitamins through Children’s Centres. Introduced a Devonwide grocery box scheme
- Continued to work with NHS and neighbouring local authorities to ensure that those who can make the most gains with regards to losing weight and stopping smoking are given every opportunity to do so, through the additional government funding for Treating Tobacco Dependence and Adult Weight Management Grant funding for 2021/22.
Recommendation 3
Continue but at pace to embed the asset-based community development (ABCD) approach to build a healthier society co-creating with communities and building on the powerful voluntary sector response to COVID. To do this, we need to make it easier for our community and voluntary sector to engage in our commissioning.
What have we done
The ABCD approach has become the established default approach to community work in Torbay. The relationships between statutory and voluntary partners have strengthened considerably in the last year not only in the COVID-19 response but beyond. One example is the cross-sectoral, community-focused response to Digital Inclusion.
Recommendation 4
Work to ensure more services recognise the importance of relationships and the impact of trauma and complexity.
What have we done
Work has progressed in the commissioning of an Alliance to meet the needs of people with complex lives. In addition, work is commencing in developing a broader, system wide approach to understanding and responding to complexity.
Recommendation 5
Work to enable people to Live Longer Better working with communities and the older person’s assembly.
What have we done
Voluntary, community and statutory organisations across Torbay have worked hard to develop pathways and services to enable people to live longer, healthier and with more independence. This work has been especially important with the increased social isolation and physical inactivity due to the pandemic. All partners are keen to ensure a strong legacy for Ageing Well Torbay. Torbay Health and Wellbeing Board have identified Healthy Ageing as a priority area for 2022-26 and partners across the system have signed up to implement the Optimal Ageing - Live Longer Better programme from 2021.
Recommendation 6
Increase and embed a focus on young people and their aspirations and their emotional and economic health as outlined in the 2019 DPH annual report and as identified as a COVID-related priority.
What have we done
Recognising the impact on emotional wellbeing that has affected all children and young people, we have focussed on our Early Help offer across Torbay.
Our wellbeing service is a partnership project working with 0 to 19, Young Devon, Checkpoint and South West Family Values. The service offers evidence-based, outcome-focused therapies for children or young people with low level mental health concerns ranging from advice and guidance in wellbeing cafés to counselling.
During the first quarter of 2020-21, there were 199 referrals to the service with 28% identifying anxiety or stress as the primary referral factor. 76% of those accessing the service felt their wellbeing had improved at the end of the sessions.
Recommendation 7
Continue to develop our mental health alliance work and to ensure a relentless focus on mental health, putting people with lived experience and the many assets in the community at the forefront of this.
What have we done
The Torbay Mental Health and Suicide Prevention Alliance have built a strong membership working together to oversee improvements in the experience of people with lived experience of poor mental health and wellbeing in Torbay. Voluntary and community partners are at the forefront of the Alliance, and some of their work programme is described elsewhere in this report.
References and further reading
- Mental Health Facts and Statistics
- NHS Outcomes Framework, 2014/15
- Department of Health; No health without mental health: A cross Government mental health outcomes strategy for people of all ages
- Chief Medical Officer’s annual report 2021: health in coastal communities
- Coronavirus and depression in adults, Great Britain
- COVID-19 mental health and wellbeing surveillance: report - Public Health England, July 2021
- Nurturing Care For Early Childhood Development, Nurturing Care Framework, 2020
- Joint Strategic Needs Assessment for Torbay 2020-2021
- THRIVE Framework
- What is Trauma-Informed Care?
- Joint Strategic Needs Assessment for Torbay 2020-2021
- Understanding Your Child, Solihull Approach
- TALKWORKS - Mental Health Support
- Torbay Self Harm Pilot Oct 21
- Chapter 6: social determinants of health
- The association between food insecurity and mental health during the COVID-19 pandemic, BMC Public Health
- COVID-19 Forecast Modelling Toolkit
- STP Two Year Report
- Public mental health and wellbeing and COVID-19 - Local Government Association
- Office for National Statistics mid-year population estimates, 2020